Pre and Post Exposure Prophylaxis (PrEP & PEP) are two essential strategies in HIV prevention, offering protection against HIV infection for individuals at different stages of potential exposure. These preventive approaches have revolutionized the landscape of prevention, providing individuals with additional tools to safeguard their sexual health.
Pre Exposure Prophylaxis (PrEP) is a daily medication taken by individuals at high risk of contracting the disease to decrease the risk of infection. On the other hand, Post Exposure Prophylaxis (PEP) is a time-sensitive treatment given after potential exposure to prevent infection. By understanding the nuances and benefits of PrEP and PEP, individuals can make informed decisions about their preventive measures based on their unique circumstances.
Why Pre Exposure Prophylaxis (PrEP) is Essential in HIV Prevention
PrEP is critical to HIV prevention, particularly for individuals with high-risk behaviors or HIV-positive partners. The primary medication utilized for PrEP involves a combination of antiretroviral drugs, including Truvada, which has demonstrated remarkable efficacy in lowering the risk of HIV transmission.
The benefits of PrEP extend beyond its effectiveness in preventing HIV infection. It empowers individuals to take control of their sexual health and make proactive decisions to protect themselves from HIV. Adhering to the prescribed regimen can significantly reduce their risk of contracting HIV, giving them peace of mind and a sense of security in their sexual relationships.
Understanding how it works is fundamental in appreciating its role in prevention. The medication works by blocking the replication of the virus in the body, preventing it from establishing a foothold and causing infection. Taking PrEP consistently and as prescribed is crucial for its effectiveness, ensuring that the medication remains active in the body to provide maximum protection against HIV.
With its proven efficacy and life-changing potential, PrEP has become a cornerstone in global efforts to reduce new HIV infections. As awareness grows and its accessibility increases, more individuals can embrace this preventive measure, contributing to the collective goal of creating an HIV-free future.
How to Access and Start Using Pre-Exposure Prophylaxis (PrEP)

Accessing PrEP involves ensuring that individuals receive the appropriate medication and support for their HIV prevention journey. The first step is to consult with a healthcare provider who specializes in prevention and is knowledgeable about PrEP. During this consultation, the provider will assess an individual’s risk factors for HIV and determine whether the drug suits them.
Once a decision is made to start PrEP, the healthcare provider will provide the necessary PrEP prescriptions and guidance on taking the medication. It is crucial to take PrEP consistently and follow the prescribed dosage to maintain its protective effect.
Finding a healthcare provider experienced in prescribing the medication is essential for a smooth and practical experience. Many healthcare facilities, community health centers, and specialized HIV clinics offer services. Additionally, some regions have online platforms and resources to help individuals find nearby providers.
Regular follow-up care is an integral part of using PrEP. Healthcare providers will conduct routine testing and monitor an individual’s overall health to ensure that PrEP remains suitable for them. Open communication with the provider is essential, allowing individuals to discuss any concerns, potential side effects, or adjustments needed for their regimen.
By taking the necessary steps to access and start using PrEP, individuals can empower themselves with a powerful preventive tool against HIV infection. Embracing PrEP as part of a comprehensive strategy contributes to more considerable efforts to curb the spread of the virus and build healthier and safer communities.
The Role of Post Exposure Prophylaxis (PEP) in Preventing Infection after Potential Exposure
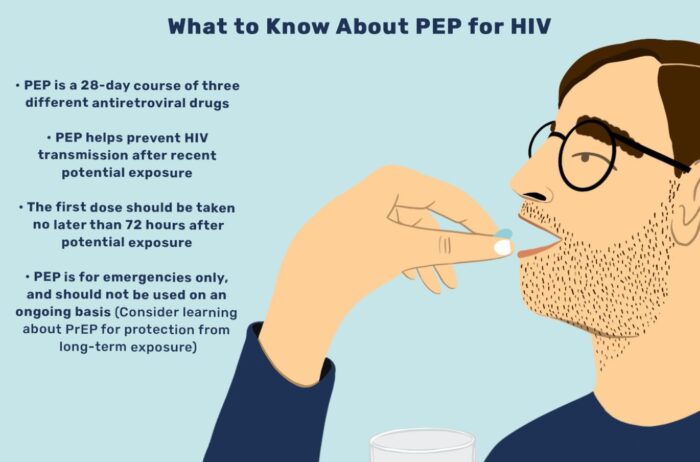
Post Exposure Prophylaxis (PEP) is a critical intervention for individuals who may have been exposed to HIV through high-risk activities or potential transmission routes. PEP involves promptly administering antiretroviral medications within 72 hours of exposure to reduce the likelihood of infection. Time is of the essence when it comes to PEP, as the effectiveness diminishes with each passing hour after the exposure.
Healthcare providers may recommend PEP in cases like incidents of sexual assault, unprotected sexual intercourse with a partner of unknown status, sharing of needles or drug equipment, or occupational exposure in healthcare settings. Individuals with condom breakage during sexual intercourse or other potential high-risk vulnerabilities may also be considered for PEP.
The effectiveness of PEP depends on timely initiation and adherence to the prescribed medication regimen. When started within the recommended timeframe, PEP can significantly reduce the risk of HIV infection. However, it is essential to remember that PEP is not 100% effective and should not replace safer sex practices or other preventive measures.
When and How to Seek Post-Exposure Prophylaxis (PEP) After Potential High-Risk Exposures

The key to PEP’s success is seeking it promptly after a potential high-risk exposure to HIV. If an individual believes they may have been exposed to HIV, taking immediate action and seeking medical attention is crucial. Ideally, PEP should be started within hours of the exposure, but it can still be considered up to 72 hours afterward, though the effectiveness decreases with each passing hour.
When seeking PEP, individuals should immediately contact their healthcare provider or visit an emergency department. Healthcare providers experienced in HIV care can assess the risk level and guide the individual through the PEP process. Emergency PEP services are available at many healthcare facilities if exposure occurs outside regular office hours.
The healthcare provider will conduct a risk assessment during the initial visit and perform baseline HIV and other relevant tests. Based on the evaluation, the appropriate PEP medication will be prescribed, and the individual will receive guidance on the dosage and duration of the treatment. The prescribed medication must be taken as directed to maximize its effectiveness.
It is crucial to remember that PEP does not replace regular preventive measures like PrEP or safer sex practices. Instead, it provides an extra layer of protection in specific emergencies. After completing the PEP course, individuals should continue practicing safer sex and consider long-term preventive options like PrEP if they are at ongoing risk for HIV.
By understanding the importance of timely PEP initiation and promptly seeking medical care after potential high-risk exposures, individuals can take proactive steps to protect themselves from HIV transmission. PEP is an essential tool in the spectrum of prevention options, offering a safety net for those who may face unplanned exposure.
The Importance of Regular Testing and Follow-Up Care for Individuals Using PrEP or PEP

Regular HIV testing and follow-up care are essential components of using Pre and Post Exposure Prophylaxis (PrEP & PEP) effectively. These preventive measures require ongoing monitoring and support to ensure their continued efficacy and individuals’ overall well-being.
For individuals on PrEP, regular HIV testing is crucial to confirm that they remain HIV-negative while taking the medication. Most healthcare providers recommend HIV testing every three months for individuals on PrEP to detect potential HIV acquisition early on. Routine testing also provides an opportunity to assess overall health, screen for other sexually transmitted infections (STIs), and address concerns related to the usage.
Follow-up care is integral to the PrEP journey, providing individuals with the necessary support and resources to adhere to their medication regimen. During follow-up visits, healthcare providers may conduct additional tests, such as kidney function and STI screenings, to monitor potential side effects or complications associated with it. Open communication between the individual and the healthcare provider ensures that any challenges are addressed promptly and that the individual feels supported in their efforts.
Similarly, individuals who have undergone PEP treatment require follow-up care to ensure that they remain HIV-negative and that the PEP regimen successfully prevents infection. Follow-up visits after PEP treatment typically include testing and may involve additional assessments based on the exposure circumstances.
Moreover, post-PEP follow-up care allows healthcare providers to discuss long-term HIV prevention strategies with the individual. For those who experienced a high-risk exposure, transitioning to PrEP may be recommended to provide ongoing protection against future disclosures.
Regular testing and follow-up care for individuals using PrEP or PEP is essential in maintaining the effectiveness of these preventive measures. Beyond testing, these visits promote overall sexual health and foster a supportive relationship between the individual and their healthcare provider. Empowering individuals with knowledge about their HIV status and offering personalized care contribute to more successful and comprehensive outcomes.
Conclusion:

In conclusion, Pre and Post Exposure Prophylaxis (PrEP & PEP) are invaluable tools in the fight against HIV and play crucial roles in protecting individuals at different stages of potential exposure. PrEP provides a proactive and effective preventive measure for those at an ongoing high risk of HIV, reducing the likelihood of HIV transmission. On the other hand, PEP offers a safety net for individuals who may have experienced potential HIV exposure, providing them with a time-sensitive opportunity to prevent infection.
By understanding the importance of timely initiation, adherence, and regular follow-up care, individuals can fully harness the benefits of PrEP and PEP. Routine testing and follow-up visits with healthcare providers ensure that these preventive measures remain effective and that individuals receive the necessary support and guidance throughout their journey.
Incorporating PrEP and PEP into comprehensive strategies fosters a world where HIV transmission is significantly reduced, and individuals are empowered to take control of their sexual health. As we expand access to these preventive measures, prioritize regular testing and follow-up care, and raise awareness about their importance, we take significant steps toward an HIV-free future. Together, we can work towards a world where HIV is no longer a public health threat, and every individual has the opportunity to lead a healthy and empowered life.